How Well Are You Managing Your Diabetes? Check Your A1C
This post was reviewed by our Director of Clinical Excellence and Oversight.
If you have diabetes, or are actively trying to avoid developing it, you’ve probably heard of a blood test called the A1C. The hemoglobin A1C test is the gold standard for measuring blood sugar because it tracks glucose over 2 to 3 months. It’s a blood test taken in the doctor’s office or clinic at any time, not necessarily on an empty stomach like some other tests.
For people with type 1 and type 2 diabetes, the A1C is like a report card that shows how well a person’s blood glucose is being managed. For those not yet diagnosed, it can reveal a blood sugar issue that needs attention.

Depending on your particular health situation, your healthcare provider will set a goal for what your A1C reading should be. Why is achieving your A1C goal so important? When blood sugar is controlled, you feel better. You also have less chance of heart disease, stroke, and other health problems. The higher the A1C, the higher the risk for complications.
The goal of this blog is to help you boost your understanding of the A1C, an extremely important metric for maintaining your health.
More Data = Better Diagnosis
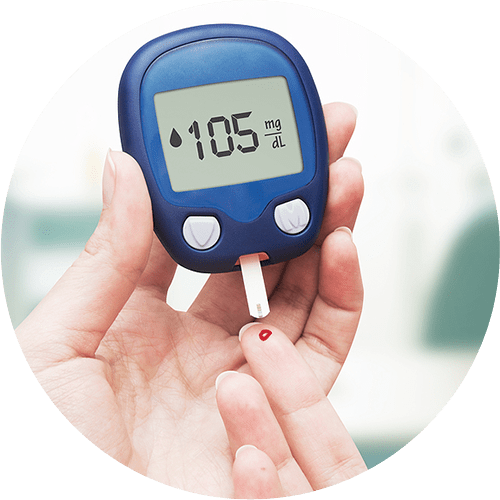
For decades, people have used fingersticks and urine tests to track their blood sugar levels. While these methods are good, they measure glucose only at the moment the test was taken. Since a person’s blood glucose levels can vary like crazy depending on the time of day, activity level, and other factors, a one-time high or low reading may not tell the whole story. That’s why the A1C is such a great tool.
How the A1C Test Works
Here’s how the A1C works. Hemoglobin is a protein found in red blood cells. Its job is to carry oxygen throughout the body. The A1C test measures what percentage of hemoglobin has glucose “stuck” to it. Hemoglobin is pretty amazing, because it maintains a record of glucose levels for about three months.
The A1C of someone with normal blood glucose is 5.6% or lower. Prediabetes is 5.7 to 6.4, and an A1C of 6.5 or higher is considered diabetes. Your doctor will recommend the ideal range for you, depending on your overall health, age, and other factors.
Continuous Glucose Monitors (CGM) and other diabetes testing products are covered by Medicare and many Medicaid, Managed Medicaid, and private insurance plans. Contact the team at HCD for more information about what your plan may include.
Where, When, and How to Take the A1C
Your doctor may recommend an A1C blood screen because you’re 45 or older, because you’re overweight, or if there’s a concern about your blood sugar. People being treated for diabetes should get an A1C at least twice a year, and more often if they change medicines, or have other health issues.
Though it’s a really good test, the hemoglobin A1C is not perfect. Factors like low iron, anemia, heavy bleeding, and kidney or liver problems can throw the reading off. Your doctor may take more than one A1C, or combine it with other tests to get the most accurate info.

Took the Test. Now What?
If your A1C is higher than your doctor wants it to be, it’s time for action. Here’s what you can do to reach your A1C goal.
Work your plan. Build any doctor-recommended changes in medicine, food, and weight loss into your diabetes action plan. If you don’t have a plan, it’s time to make one with the help of your care team. A good plan includes everything from your emergency contacts and medication list, to target glucose levels and meal notes.
Watch your diet. Choose fewer carbs and starchy vegetables and more salads, green vegetables, and low-fat protein and dairy products. Try to break the habit of reaching for that processed, frozen meal and start to cook, even a little. Fad diets rarely work, but eating more whole, plant-based foods is a smart long-term strategy.
Beware of bogus beverages. Make water, unsweetened coffee and tea, vegetable juice, and low-fat milk your drinks of choice. Juice and soda can have as much as 9 teaspoons of sugar in an 8-ounce serving. Although diet sodas don’t have calories, the artificial sweeteners have been linked to some health problems.
Move more. You’ve heard it before, but we’re here to tell you again! Regular exercise can help reduce your blood sugar. The more muscle, the more sugar you burn. So, stay on that exercise program, and tweak it if necessary. If you’ve fallen off the wagon, it’s time to get up and get moving. Any exercise is better than none. A 10-minute walk is a great way to start! Unless your doctor says otherwise, try for 150 minutes of exercise a week.
Know your numbers. Testing your blood tells you if the steps you’re taking to reduce your A1C are working. If you use a Continuous Glucose Monitor (CGM), you’re getting readings 24/7. If you test by fingerstick, talk to your healthcare team about testing more often, at least for a while. Chart your findings and compare them to your goal.
While general guidelines will help most people, the ideal balance of food, activity, and medication is something you and your care team will discover together. Learn all you can, and do all you should, to achieve an A1C that will keep you healthy and avoid complications.
Mindfulness Helps
When it comes down to it, managing A1C is as individual as you are. While general guidelines will help most people, the ideal balance of food, activity, and medication is something you and your care team will discover together. Learn all you can, and do all you should, to achieve an A1C that will keep you healthy and avoid complications.
Be mindful of the emotional part of all this. Diabetes is a chronic disease—that means you’ll likely have it, and have to manage it, for a long time. You may want to join a diabetes support group online or in person. Or you might have a friend or family member with diabetes who could be a good sounding board. Or you may need to take a little bit of time every day to meditate or take stock of how you are feeling and managing all the parts of your care plan.

HCD Is Here for You!
Also essential in managing your diabetes are the monitoring supplies and other insurance-covered products you can get from HCD. Whether you use a traditional method to test your blood glucose—lancet, test strip, and meter—or have switched to a Continuous Glucose Monitor (CGM), Home Care Delivered is your one-stop shop.
Beyond the great products, we also deliver the absolute best in customer service. Our customer service team is as personal and hands-on as it gets. We even have a Certified Diabetes Care and Education Specialist (CDCES) as part of our Clinical Team. Give us a call at 866-938-3906 or visit supplies.hcd.com/cgm. We’re right here, ready to tackle your diabetes management with you!

Get Insurance-Covered CGM & Diabetes Supplies
Monthly Deliveries | We Handle the Paperwork

Disclaimer:
Unless otherwise noted, the recommendations in this document were obtained from the sources indicated. Be advised that information contained herein is intended to serve as a useful reference for informational purposes only. HCD cannot be held responsible for the continued accuracy of or for any errors or omissions in the information. All trademarks and registered trademarks are the property of their respective owners.

