Medicare vs. Medicaid: Which One Do I Have?
This post was reviewed by our Director of Clinical Excellence and Oversight.
The differences between Medicare and Medicaid are not simple. Each has many different plan options, including: Fee-For-Service, QMB, SLMB, Managed Care, and QI. So how do you know which one you have?
This guide will help you learn the differences between Medicare and Medicaid, along with how to learn which you have.
Skip to a Topic:
Medicare vs Medicaid
Medicare Vs. Medicaid: What’s The Difference?
There are three major differences between Medicare and Medicaid: Who provides it, who can qualify, and how it’s structured. Here’s a breakdown of each:
Medicare
Provided by the federal government to people who:
- Are age 65 or older
- Are under age 65 with certain disabilities
- Have End-Stage Renal Disease
Structure: Divided into 4 parts
Part A Part B
Part C Part D
Medicare
Provided by individual states to people who meet at least one of these categories:
- Have lower incomes
- Are blind or disabled
- Receive Supplemental Security Income (SSI)
- Are pregnant and need assistance
- Are disabled but working
Structure: Offered through Fee-For-Service or Managed Care plans.
About Medicare
Medicare is a national health program provided by the US government. It’s divided into 4 parts: Part A, Part B, Part C, and Part D.
Every American who paid into Medicare is automatically enrolled in Part A and Part B when they turn 65. People under 65 with certain disabilities may also apply to enroll.
Parts of Medicare
Part A – Covers time spent in a health facility such as a hospital, hospice care, or home health agency.
Part B – Covers health expenses such as doctor visits, surgery, medical supplies, lab work, and test screenings.
Part C – A combination of Part A and B that can also include dental, vision, prescriptions, and other health services.
Part D – Covers prescription drugs.
Medical Supplies Covered by Medicare
The following medical supplies could be covered by Medicare, depending on individual needs:
Urology Supplies – Catheters, insertion kits, lubricant, condom catheters, & more.
Diabetic Supplies – Test strips, blood glucose monitors, lancets, test solution, & more.
Ostomy Supplies – Skin barriers, 2 piece pouch systems, drainage bags, & more.
Wound Care Supplies – Bandages, foam dressings, tape, gauze, hydrogels, & more.
Note: Medicare does not cover absorbent incontinence supplies.
How Do I Know If I Have Medicare?
Since Medicare is a national program, all Medicare insurance cards look the same. Here’s an example:
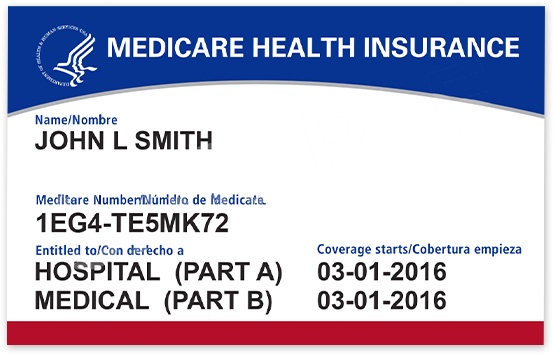
People with Medicare Advantage will have two insurance cards: One for traditional Medicare, and one for their Medicare Advantage plan. Medicare Advantage cards will look different from each other, depending on the plan.
About Medicaid
Medicaid is a health program provided by individual state governments to people who meet at least one of the income or disability requirements.
Nobody is automatically enrolled in Medicaid. To receive it, you must apply through your state’s Medicaid office.
Types of Medicaid
There are two basic types of Medicaid: Fee-For-Service and Managed Medicaid.
Fee-For-Service – Medicaid pays doctors, hospitals, and other healthcare providers for the individual services or products received by the Medicaid member.
Managed Medicaid (Managed Care Plan) – The state contracts with a private insurance company to manage and administer Medicaid benefits. Member benefits will be similar to fee-for-service, but could vary depending on the plan.
Get Incontinence Supplies Online With Medicaid
No Credit Card | Fast Delivery | 100% Discreet
Supplies Covered by Medicaid
The following medical supplies could be covered by Medicaid, depending on the state and the individual plan:
Incontinence Supplies – Bladder control pads, pull-on underwear, adult briefs, & more.
Urology Supplies – Catheters, insertion kits, lubricant, condom catheters, & more.
Diabetic Supplies – Test strips, blood glucose monitors, lancets, test solution, & more.
Ostomy Supplies – Skin barriers, 2 piece pouch systems, drainage bags, & more.
Wound Care Supplies – Bandages, foam dressings, tape, gauze, hydrogels, & more.
What Type of Medicaid Do I Have?
Knowing which kind of Medicaid you have can be tricky. Every state has its own Medicaid program, which means coverage, requirements, and Medicaid cards will vary. The best way to know which one you have is to call the number on the back of your insurance card.
Having Both Medicare and Medicaid
In some cases, it’s possible for someone to have both Medicare AND Medicaid. In order to enroll in both programs, the individual must meet the eligibility requirements for both programs.
Medicare Savings Program
Eligible Medicare members can enroll in a Medicare Savings Program (MSP). These provide financial assistance for Medicare costs, such as premiums, deductibles, and coinsurance.
Generally, people with an MSP only receive Medicare benefits. Some, however, may also be eligible for Medicaid benefits.
Types of Medicare Savings Programs: QMB, SLMB, & QI
There are many different programs available, including but not limited to: Qualified Medicare Beneficiary (QMB), Specified Low-Income Medicare Beneficiary (SLMB), and Qualifying Individual (QI).
Qualified Medicare Beneficiary Only (QMB)
Qualified Medicare Beneficiary Only (QMB) is a Medicaid-funded program that provides financial assistance to cover Medicare Part A and Part B premiums. It also covers Medicare deductibles, coinsurances, and copays.
This program does not cover medical supplies. For example, someone with QMB cannot use it to receive incontinence products.
Qualified Medicare Beneficiary Plus (QMB+)
Qualified Medicare Beneficiary Plus (QMB+) offers the same benefits as QMB Only except for one big difference: People with QMB+ also have full Medicaid benefits.
This means that people with QMB Plus may be eligible to receive supplies through Medicaid. Coverage and plan availability will vary by state. To find out if you have QMB Plus, call the number on the back of your insurance card.
Specified Low-Income Medicare Beneficiary Only (SLMB)
Specified Low-Income Medicare Beneficiary Only (SLMB) is a Medicare program that helps people afford the insurance premium of Medicare Part B only. Like the QMB program, recipients must apply through their state Medicaid office to determine eligibility.
This program does not cover supplies; it only covers the Medicare Part B premium. For example, someone with SLMB Medicaid cannot use it to receive incontinence products.
Specified Low-Income Medicare Beneficiary Plus (SLMB+)
Specified Low-Income Medicare Beneficiary Plus (SLMB+) provides the same financial help as SLMB Only. The difference is that people with SLMB+ also have full Medicaid benefits.
This means that people with SLMB+ may be able to receive medical supplies through Medicaid. Product coverage and plan availability will be different for each state. To find out if you have SLMB+, call the number on the back of your insurance card.
Qualifying Individual (QI)
Just like the SLMB, the Qualifying Individual (QI) program is a program that helps people cover the premium of Medicare Part B only. People with QI, however, do not qualify for Medicaid.
This program does not cover supplies; for example, someone with QI Medicaid will not have incontinence supplies covered.
Extra Help
Medicare recipients who qualify for QMB, SLMB, or QI programs automatically qualify for Extra Help. The Extra Help program is designed to reduce the cost of prescription drugs for participants.
To learn more about Extra Help, visit Medicare’s Extra Help Guide.
How Do I Know If I Have a Medicare Savings Program?
Just like Medicaid, MSPs can be tricky. Since Medicaid handles MSPs, the cards and programs available may vary by state. The best way to know is to call the number on the back of your insurance card.
Getting Medical Supplies with Your Insurance
Now that you know which insurance you have, contact us to find out what supplies you can get with your benefits.
We can tell you exactly what insurance benefits you have and what supplies they cover. We can also set you up with monthly orders delivered right to your door.
Here’s how it works:
- You provide us with some basic information.
- We work with your insurance and doctor to collect the paperwork.
- Once complete, we’ll send you monthly deliveries of supplies.

We’ll also make sure you’re using all the benefits you qualify for, so you don’t pay more than you should for supplies.
If you have Medicare or Medicaid, contact us today to see what supplies you could get with your benefits.
Medical Supplies Delivered to Your Door
Accurate Orders | Fast Delivery | Product Expertise

Disclaimer:
Unless otherwise noted, the recommendations in this document were obtained from the sources indicated. Be advised that information contained herein is intended to serve as a useful reference for informational purposes only. HCD cannot be held responsible for the continued accuracy of or for any errors or omissions in the information. All trademarks and registered trademarks are the property of their respective owners.

